Today’s hook
Have you ever felt a physical tightness in your chest when you see someone get hurt? Or found it hard to watch painful scenes in movies—or even in surgery videos?
Today’s science is saying: that’s not “being dramatic.” It’s empathic pain—and it has its own circuitry in the brain, with real therapeutic potential.
The paper I’m bringing today, published in Neuropharmacology in 2025, maps in detail the neural circuits and therapeutic mechanisms behind empathic pain. (PubMed+1)
The authors combine human neuroimaging findings with rodent models and land on two strong messages:
- Empathic pain involves a well-defined circuit—it’s not just “imagination.”
- Modulating this circuit could help both psychiatric conditions with empathy deficits (autism, psychosis, schizophrenia) and chronic pain management. (PubMed+1)
The simplified deep dive
1) What is empathic pain in practice?
The authors define empathic pain as the experience of “feeling” another person’s pain, with activation of circuits similar to those involved in one’s own pain—even without any real tissue damage. (ScienceDirect+1)
Key points:
This response includes three dimensions:
- Sensorimotor: your body prepares; you flinch, tense up, look away
- Affective: distress, compassion, discomfort
- Cognitive: rationally understanding what the other person is going through (ScienceDirect)
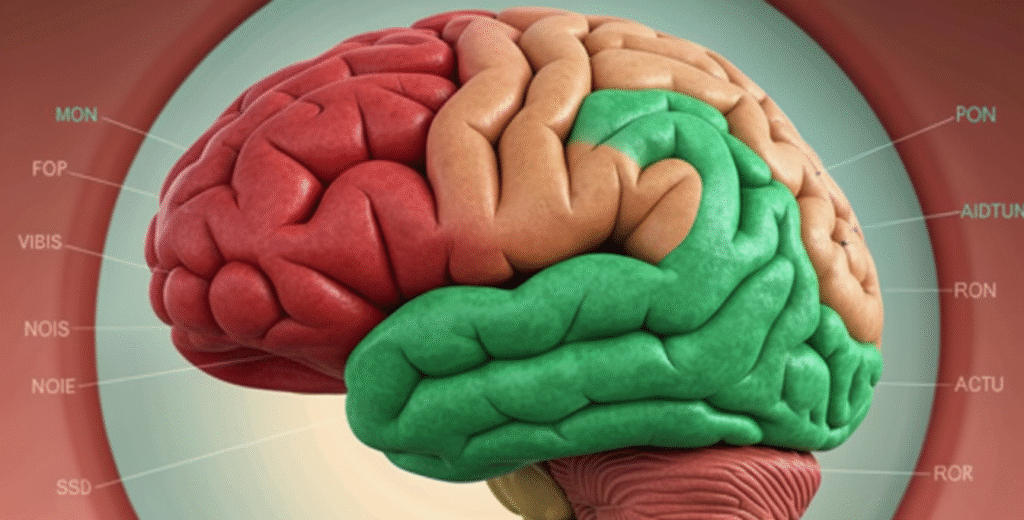
fMRI studies show that when we watch someone else in pain, we activate regions from the so-called “pain matrix,” especially:
- the anterior cingulate cortex (ACC)
- the anterior insula
- the amygdala, and even the cerebellum in some studies (ScienceDirect+1)
An analogy I like: empathic pain is like emotional Wi-Fi—the other person’s body is the router, and your brain picks up the signal in pain, emotion, and decision-making networks.
2) The fine circuitry: from the locus coeruleus to the striatum
The most “nerdy” (and fascinating) part of the paper is how it details the circuitry. In animal models of empathic pain—where a “demonstrator” rodent is in pain and an “observer” watches—the authors highlight specific connections: (ScienceDirect+1)
- LC → mPFC (locus coeruleus to medial prefrontal cortex)
A noradrenergic pathway linked to vigilance, attention to threat, and stress responsiveness. - ACC → NAc (anterior cingulate to nucleus accumbens)
Integrates pain, motivation, and reward—helping explain why relieving someone else’s pain can feel “rewarding” and promote prosocial behavior. - IC → BLA (insula to basolateral amygdala)
Links visceral/affective sensation with emotional memory of fear and threat. - VTA → NAc and VTA → LHb (ventral tegmental area to accumbens and lateral habenula)
Classic reward/aversion circuits that modulate whether another person’s pain feels unbearable or tolerable. (ScienceDirect)
In clinic language:
Empathic pain starts in a social–sensory circuit (seeing/knowing another person is suffering), passes through emotion and memory hubs, and ends in motivation and decision centers—biology that pushes us to help, avoid, flee, or freeze.
3) When empathy is blunted—or overwhelming
The paper connects these circuits to disorders where empathy is altered: (PubMed+1)
Autism
- Difficulties reading and responding to others’ emotional states
- Studies show atypical activation patterns in empathy/pain networks
Psychosis and schizophrenia
- Changes in theory of mind and cognitive empathy
- Possible hypo- or hyperactivation in ACC, insula, and amygdala circuits
Other conditions with distorted empathy (like some personality disorders) also come up, though the paper focuses more on major neuropsychiatric groups.
An interesting point: the authors suggest that modulating empathic pain—up or down—could help treat core symptoms in these populations, for example:
- increasing empathic sensitivity in people with deficits
- reducing empathic overload in those who absorb too much suffering and burn out—like some healthcare workers (PubMed+1)
4) What are the therapeutic possibilities?
The review discusses multiple strategies that target these circuits: (PubMed+1)
Targeted neuropharmacology
Noradrenergic (LC→mPFC), dopaminergic (VTA→NAc), glutamatergic targets, and neuropeptide modulators could, in theory, recalibrate empathic responsiveness—still largely in the preclinical stage.
Noninvasive neuromodulation
TMS and tDCS targeting ACC, mPFC, and insula are cited as promising routes to regulate empathic pain and emotion networks—consistent with what we’re already seeing develop in depression, chronic pain, and PTSD.
Behavioral interventions
Empathy, compassion, and emotion-regulation training likely act on these same networks in a top-down way—though stronger, more standardized protocols plus paired functional imaging are still needed.
And there’s one especially elegant idea: using empathic pain science to treat physical pain.
The logic:
- chronic pain isn’t just peripheral input
- it involves negative emotion, social isolation, and constant interpretation of pain—others’ and one’s own
- if we understand how the brain encodes and regulates others’ pain, we can design therapies that reduce subjective suffering even without fully “zeroing out” peripheral signals (PubMed+1)
Implications and invitation
What do I take from this paper into practice—and into conversations with patients and teams?
Empathy isn’t only a moral virtue—it’s neurobiology.
That helps move the conversation away from blame (“you’re cold,” “you feel too much”) and toward: “your brain is tuned this way—and we may be able to retune it.”
Empathic pain is a bridge between psychiatry and chronic pain.
Strategies that strengthen connection, social support, and emotion regulation aren’t fluff—they directly engage ACC, insula, amygdala, and striatal networks.
Near future: treatments that target empathy as a therapeutic endpoint.
From more specific drugs to TMS protocols and compassion-training programs, the trend is for empathy to move out of philosophy and into formal clinical intervention.
My personal takeaway: understanding empathic pain is understanding why suffering is contagious—and how we might use that contagion to support healing instead of burnout.
That was today’s dose of science in the Medical Innovation column.
Now I want to hear from you: in your practice, do you see more people who are “numb” to others’ pain—or more professionals and families burned out from too much empathic pain? How do you imagine using this kind of knowledge day to day?
Source:
Yang Z, Xie L, Zhang B, et al. Neural circuits and therapeutic mechanisms of empathic pain.